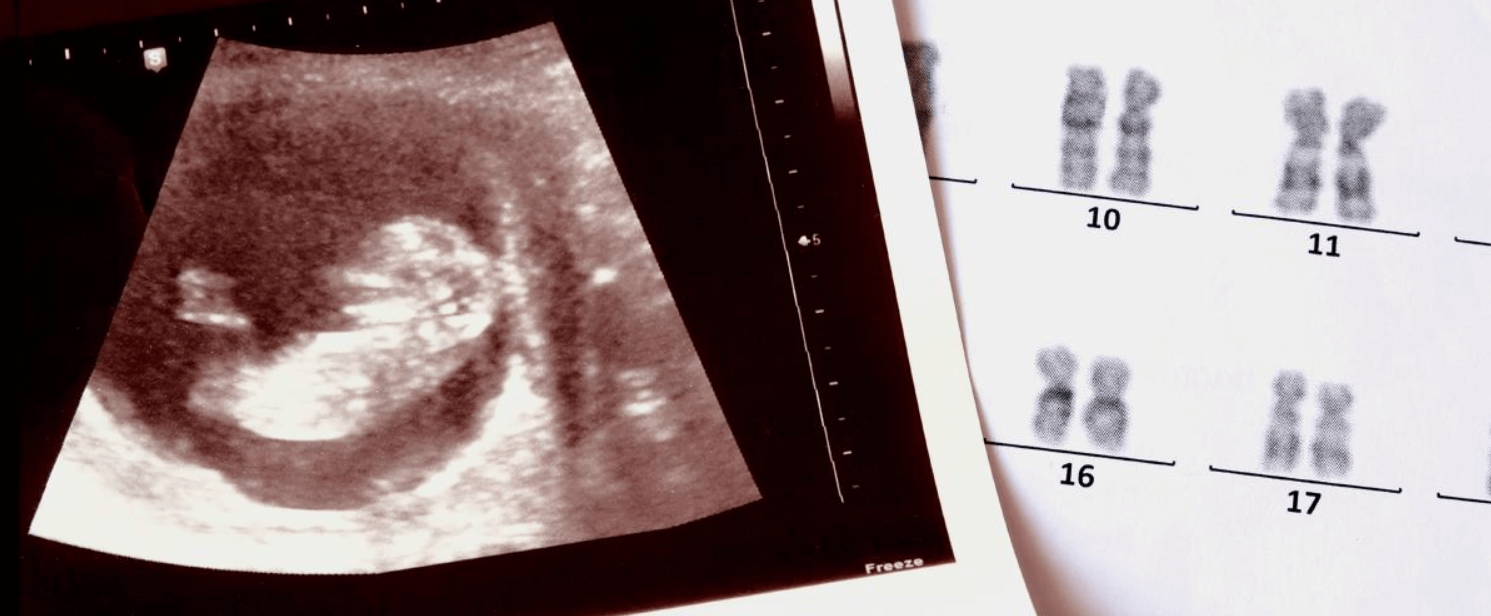
The spectrum of information that can be obtained by prenatal testing is wide and rapidly increasing. Many mutations, or "abnormalities," are inconsequential, while others are significant.
I became interested in anomalies of the human sex chromosomes, X and Y, as a medical student. I had a patient with a rare genetic condition that gave rise to a syndrome once referred to as male pseudo hermaphroditism and now called "androgen insensitivity syndrome" (AIS) or "testicular feminization." This intersex condition is caused by either of two types of mutation on the X chromosome. (Recall that females are generally XX, while males are XY.)
So, while normally people with one X and one Y chromosome in every somatic cell (who are designated "XY") would be males, an inherited mutation distorts development. One mutation causes a deficiency of the receptor for the hormone dihydrotestosterone (DHT), which promotes male characteristics; in the other, the receptor is present, but the receptor-DHT complex is inactive. In either case, the hormone cannot perform its normal actions which would give rise to a male-appearing fetus.
One well-known example of someone with this condition is Caster Semenya, a South African two-time Olympic champion and three-time world champion over 800 meters. Between 2009 and 2019, she won 30 consecutive middle-distance races. Although she has identified as female her whole life, she is biologically male, her sexual organs shaped by AIS. Her internal testes produce naturally high testosterone levels in the typical male range.

My med school patient was genetically male (XY) but because of the mutation, his cells were unable to respond to DHT in utero, the result of which was the birth of a person who became a normal-appearing woman with adequate breast development, normal female external genitalia but a vagina of less than normal depth, absent uterus, sparse pubic and axillary hair, and the absence of menstrual periods.
(These situations add a new wrinkle to the current confusion about appropriate pronouns.)
Some form of testicular feminization occurs in about one out of 20,000 births and can be incomplete (giving rise to various sexual ambiguities) or complete (the genetic male appears to be a woman). Even many physicians have never heard of it, so I was surprised to see a case of it depicted several years ago on the British TV series, "Call the Midwife," in which one of the characters, Lois Parry (shown below), discovered that she was intersex. There is a description of the episode here.

Testicular feminization is the kind of abnormality that can be detected by prenatal genetic tests, which raises various medical, ethical, and moral issues because there is currently no treatment for it.
Far more common are variations in sex chromosomes where people have an extra or missing entire X or Y. They are the most frequent chromosomal anomalies, occurring in approximately one in 400 births. However, most people affected are unaware that they have them because the anomalies are not life-disrupting and, unlike testicular feminization, seldom give rise to telltale characteristics, signs or symptoms. Because of the confusion and anxiety that can ensue when a person learns of his or her genetic anomaly, this might be one of those cases in which knowing about the diagnosis might be worse than the "disease" itself.
The first noninvasive prenatal screening (NIPS) appeared just over a decade ago. The first-trimester blood tests that became available in 2011 to detect Down syndrome have vastly expanded their repertoire, gradually adding more conditions, including atypical numbers of sex chromosomes, to their panel.
In 2020, the American College of Obstetricians and Gynecologists endorsed conducting noninvasive prenatal screening during all pregnancies. Their website describes the various categories of genetic disorders that may arise:
Aneuploidy is a condition in which there are missing or extra chromosomes. In a trisomy, there is an extra chromosome. In a monosomy, a chromosome is missing. Inherited disorders are caused by changes in genes (mutations). Inherited disorders include sickle cell disease, cystic fibrosis, Tay-Sachs disease, and many others.
Testicular feminization is in the last category – mutations that give rise to abnormalities.
Although parents-to-be might think the test is intended primarily to rule out Down syndrome or more severe abnormalities, as noted above other findings might be detected, many of them inconsequential. Even so, the finding of sex chromosome abnormalities often precipitates a decision to terminate the pregnancy, particularly in younger couples.
Given the complexity and importance of the information derived from prenatal testing, parents-to-be would be wise to obtain genetic counseling to provide information about how genetic abnormalities might affect them and their family, if at all. The genetic counselor (or other qualified healthcare professional) collects personal and family health history which is used to estimate how likely it is that the fetus has a serious genetic condition and to recommend which genetic tests might be appropriate.
This is truly a situation in which, as the saying goes, knowledge is power. Expectant parents should obtain counseling to learn what the future may hold.
Henry I. Miller, a physician and molecular biologist, is the Glenn Swogger Distinguished Fellow at the American Council on Science and Health. He was the founding director of the FDA's Office of Biotechnology. Find Henry on X @HenryIMiller

